This story was part of Healthbeat’s live storytelling event, “Aha Moments in Public Health,” held Nov. 18 at Powerhouse Arena bookstore in Brooklyn. Watch the full show here. Sign up to receive Healthbeat’s free New York newsletter here.
What matters most in health care goes beyond medical treatment. It is understanding what truly matters to each person and shaping care around their lives, not just their diagnoses. I learned this lesson firsthand in 2020, when I had just graduated from medical school, moved to the United States, and began my journey caring for some of New York City’s most vulnerable older adults through my work at JASA, one of the city’s largest providers of aging services.
In medical school, I was trained to treat disease and preserve health, yet I quickly realized how little I knew about what happens once patients leave the hospital. Social determinants, daily challenges, and loneliness can profoundly affect recovery and quality of life.
In 2021, I met a patient I will call Mr. Happy. He had recently been discharged after a prolonged hospitalization for congestive heart failure exacerbation and ascites secondary to colon cancer. Reaching him was difficult since he was often unavailable, and the referring social worker warned me that he was hard to engage. When I finally did, he became both my teacher and my patient.
My first “aha” moment came when Mr. Happy taught me the power of patience and persistence. After several attempts, he finally agreed to a visit. When I arrived, I immediately understood his hesitation. His apartment was nearly empty. During his hospitalization, his few possessions had been discarded. He had no chair, no linens, no clothes. He was angry and embarrassed. Through JASA’s support, I was able to provide clothing, shoes, linens, and a recliner so he could sit comfortably.
As we reviewed his medications, I discovered that he had stopped taking his heart failure medicine because it was unaffordable without insurance. I contacted the manufacturer, obtained a coupon, and coordinated with his pharmacy. Within hours, he had his medication in hand. We reviewed each prescription together using the teach-back method and created a simple list he could follow. From that point forward, he took his medications consistently. That was my second “aha” moment: realizing that patients often labeled as “non-compliant” are, in fact, navigating real and significant barriers to care.
My final “aha” moment came when JASA implemented the Age-Friendly Health System framework, which centers on asking every patient a single, transformative question: “What matters most to you?”
That question changed my entire approach to care. For Mr. Happy, what mattered most was regaining his health so he could spend time with his son and siblings and once again play chess in the park. Together, we worked to make that possible by arranging transportation, medication delivery, and home aide support, and by helping him secure insurance for ongoing care.
Through this experience, I learned that true healing begins when we listen deeply to what matters most. Mr. Happy became more than a patient; he became a mentor. On my final visit, we played chess together, honoring one of the things that mattered most to him. He reminded me that compassionate, person-centered care, grounded in empathy and partnership, is at the heart of medicine.
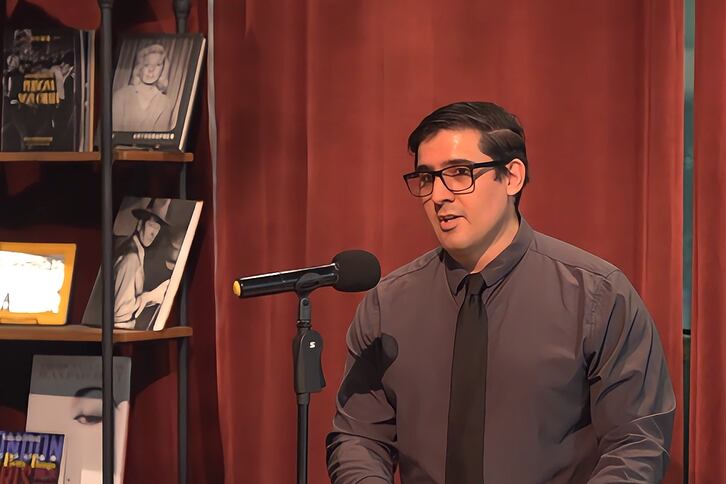
Dr. Jose R. Martinez-Escudero is the associate director of transitional care for JASA at Maimonides Hospital, where he helps underserved older adults navigate the complexities of the health care system in New York City. Dr. Martinez-Escudero completed his medical training at the National Polytechnic Institute in Mexico City, followed by a Master of Science degree focused on research in Parkinson’s disease and the basal nuclei.