This article originally appeared at Your Local Epidemiologist New York. Sign up for the YLE NY newsletter here. Public health, explained: Sign up to receive Healthbeat’s free New York City newsletter here.
Is it just me, or does it all of a sudden feel like fall in New York this week? And I am all for it 🍁 There’s a lot to cover this week, so let’s jump right in.
Infectious disease ‘weather report’
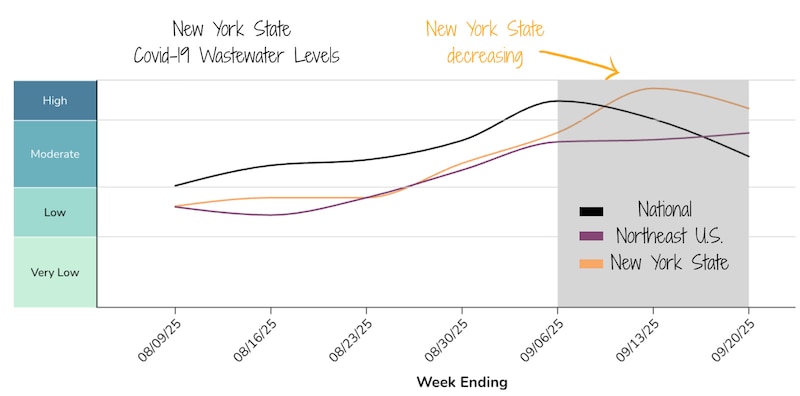
Covid-19: Declining, but still elevated.
RSV: No activity yet in New York.
Flu: No activity yet in New York.
During this lull is the perfect time to get vaccinated — before respiratory viruses pick up.
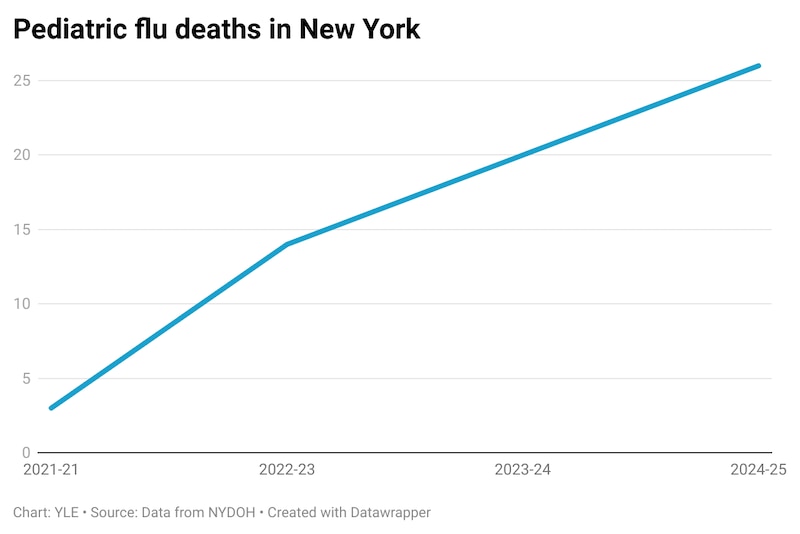
A new Centers for Disease Control and Prevention report underscores why. Last flu season was especially severe, with one of the highest numbers of pediatric flu deaths in recent years. Nationwide, 109 children developed influenza-associated encephalopathy, a dangerous brain swelling caused by flu infection. In New York alone, 26 children died. And pediatric flu deaths here have been increasing.
Now is the time to get vaccinated and reduce the risk of severe infection. Katelyn Jetelina at YLE National wrote an excellent fall vaccine primer to help you navigate decisions.
Measles detected in Oswego County wastewater
The New York State Health Department issued an alert after measles was detected in wastewater in Oswego County. (The Wastewater SCAN group is testing for measles in Oswego and Ithaca, and New York City is running their own measles testing program.) This means there is at least one case in the community, even though no infections have been identified yet. The alert is to remind health care providers to stay alert for signs and symptoms of measles in patients.
Because measles is so contagious, you need ~93-95% of the population to be vaccinated to prevent an outbreak. In Oswego County, 87.8% of kids under 2 are vaccinated, leaving some susceptible to infection. In response, the health department is monitoring for cases.
The actual risk of an outbreak depends on the community surrounding the person infected. If the person shedding the virus is in a community with high vaccination rates, the risk is low. But if they’re in a pocket with lower coverage, the chance of spread is higher.
For now, no cases have been identified. I’ll be keeping a close eye on this.
For the public, the guidance hasn’t changed: Vaccination is the best protection. For more details, here are common FAQs on the measles vaccine from YLE National.
Measles symptoms usually start like a cold or flu (fever, cough, runny nose, etc.). A rash typically appears a few days later. If you’re sick and think you may have measles, call ahead before going to a clinic, urgent care, or ER so infection-control precautions can be taken.
Chikungunya in Long Island and a death due to EEE
Last week, a woman in Long Island tested positive on a preliminary screen for chikungunya, a virus spread by certain species of mosquitoes. What makes this case unusual is that she had no recent travel history. (Occasionally, travelers will return to New York after acquiring chikungunya abroad.) The New York State Health Department is running additional tests to confirm. If confirmed positive, this would be the first locally acquired case in New York.
Chikungunya is very rare in the United States. The last locally transmitted cases occurred in 2015, with small outbreaks in Florida and Texas. Globally, it’s much more common, particularly in the Caribbean and South America, and a major outbreak is ongoing in China this year.
Symptoms include:
- Fever
- Severe joint pain or swelling
- Headache
- Muscle pain
- Rash
Why now? Evidence shows that climate change is expanding and shifting the range of the mosquitoes that can carry chikungunya. More frequent human travel and global shipping also help mosquitoes spread, as they can hitch rides on planes, boats, and even in luggage. While we won’t ever know if climate change directly caused this single case, it likely played a role. Epidemiologist Colin Carlson broke down how climate change may be:
- Allowing the mosquito to survive in New York
- Creating warmer conditions that support viral replication within mosquitoes
- Driving larger global outbreaks, increasing the chance of introduction here in New York
As we move into fall and temperatures drop, the risk of more local cases decreases. The overall chikungunya risk in New York remains very low, but we’re still in mosquito season, so it’s best to avoid bites. Wear repellent (Deet or picaridin) or long sleeves, especially at dawn and dusk when mosquitoes are most active, and dump standing water around your home.
Sadly, the case of Eastern Equine Encephalitis virus we covered last week has died. We are sending our love to his family and loved ones.
CTE was confirmed in man who shot and killed four in Midtown NYC office building
Public health goes beyond microbes. Understanding the drivers of violence, and especially gun violence, is incredibly important in the United States.
The man who shot and killed four people in a Midtown Manhattan office building in July was found to have chronic traumatic encephalopathy during an autopsy. CTE is a degenerative brain disease caused by repeated head trauma and is seen most often in athletes and military veterans. It’s linked to impulsivity, depression, memory loss, cognitive decline, and suicidal thoughts. It can only be definitively diagnosed after death.
In a letter, the gunman claimed he developed CTE from playing football. He said his attack was directed at the NFL headquarters and claimed they hid the effects of CTE.
Did CTE cause the shooting?
We won’t ever know whether CTE fully explains this violent act, or if it was just one piece of a more complex picture involving mental health. The truth is, the link between CTE and violence isn’t well understood. One big reason is selection bias. Most brains studied for CTE are from people who showed noticeable symptoms or were involved in high-profile acts of violence. That means we’re missing the full picture. Many people may live with CTE without ever being violent.
CTE isn’t just about concussions
Research shows it’s the cumulative number and intensity of head impacts, not just concussions, that increase risk. Even minor hits, repeated over time, can damage brain cells and blood vessels, leading to microscopic bleeding and toxic protein build-up in the brain.
Prevention starts early
Changing how kids practice football, like reducing full-contact drills or encouraging flag football, can dramatically reduce risk. The Concussion Legacy Foundation estimates that a high school offensive lineman averages 734 head impacts a season with an average strength of 26 g. Because most hits occur in practice, if the number of practice hits were cut in half, like by switching to flag football from some drills, it could cut the overall number of head impacts kids experience by about a third. The fewer and softer the hits, the safer the brain.
Because CTE is only diagnosed after death, it’s incredibly hard to study, and many research gaps remain. But given the possible links to violence and severe mental health issues, it’s an urgent public health priority.
If you or someone you love is struggling after repeated head trauma, resources and help are available: The CDC’s Heads Up Program and the Concussion Legacy Foundation HelpLine can provide resources to those at risk of or struggling with brain injury.
CDC wants to know how you feel after vaccination
V-safe is a vaccine safety monitoring system that lets you tell CDC how you feel after vaccination by completing check-ins. It was created to monitor the safety of Covid-19 vaccines and has expanded to include RSV vaccines. The data collected through V‑safe helps the CDC communicate timely, transparent information about the safety of vaccines. You can sign up here to complete short check-in surveys by text or email following your vaccine.

Bottom line
You’re all caught up on New York health news! Now is the time to get fall vaccines before things start picking up again. See you next week, and I hope you enjoy this changing season!
Love,
Your NY Epi
Dr. Marisa Donnelly, PhD, is an epidemiologist, science communicator, and public health advocate. She specializes in infectious diseases, outbreak response, and emerging health threats. She has led multiple outbreak investigations at the California Department of Public Health and served as an Epidemic Intelligence Service Officer at the Centers for Disease Control and Prevention. Donnelly is also an epidemiologist at Biobot Analytics, where she works at the forefront of wastewater-based disease surveillance.