Public health, explained: Sign up to receive Healthbeat’s free Atlanta newsletter here.
While Georgia has had relatively few Covid and influenza cases this fall, data from the Centers for Disease Control and Prevention indicate that respiratory syncytial virus, also known as RSV, recently peaked at the state’s highest levels in years.
Numbers from late November indicate state hospitalization rates for the virus were the highest they’ve been since at least fall 2018, according to the CDC’s Respiratory Virus Hospitalization Surveillance Network. Wastewater sampling, which can be used to detect some infectious disease levels in localities, also reveals that there have been high amounts of RSV circulating in Fulton, Muscogee, and Chattahoochee County communities.
These trends are distinct from RSV levels in the rest of the country. For the United States as a whole, data suggest infection levels are rising but not yet approaching peaks in 2022 or 2023.
Georgia’s recent relative RSV increase is higher than previous markers, but visits for the virus haven’t surpassed 1% of hospital visits in a sample of eight CDC-monitored Georgia hospitals. In comparison, flu visits accounted for about 8% of visits at these sites last December.
Hospitalization counts can lag behind testing data, and the most recent preliminary CDC data show that in-patient RSV stays are decreasing in Georgia. Emory Director of Pulmonary and Critical Care Medicine Dr. Greg Martin said his system’s testing data also indicate cases have declined over the past two weeks. He said influenza cases appear to be on the rise after a more limited Georgia spread compared to the last two flu seasons.
This year’s flu vaccine, which is expected to provide an extra layer of protection from severe disease, appears to be embraced by most Georgia residents. A CDC survey from late November found that about 67% of adults in the state said they either have or intend to get a flu shot for this season. About 71% of Georgia parents said their kids are or probably will be vaccinated this season — about 6% higher than the national average.
That’s significantly lower than plans for the updated Covid-19 shot. The same survey noted that about half of Georgia adults plan to get or have gotten that vaccine, and only about 42% of parents are taking those steps for their children. Both responses are about 6% lower than the United States as a whole, respectively.
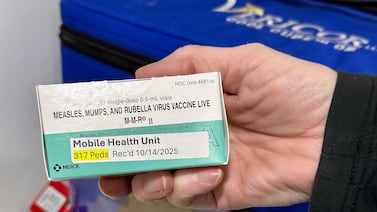
The CDC only recommends certain groups — seniors over 70, adults over 60 at high risk of severe symptoms, and infants under 8 months old — receive a vaccine that protects people from RSV. An October CDC survey showed that over 90% of U.S. infant parents said they had gotten or plan to get their babies immunized against RSV, and 76% American adults in recommended groups said they have received or intend to get the shot.
In contrast, 67% of adults in those high-risk categories living in a group of southeastern states, including Georgia, said they have done or plan to do the same.
Allen Siegler is a reporter covering public health in Atlanta for Healthbeat. Contact Allen at asiegler@healthbeat.org.