This article originally appeared at Your Local Epidemiologist New York. Sign up for the YLE NY newsletter here. Public health, explained: Sign up to receive Healthbeat’s free New York City newsletter here.
One night last fall, I stood at my kitchen sink in New York City, filling a water bottle from the tap. I had just read a local report about lead pipes in Syracuse that, in some neighborhoods, are still directly connected to homes. I kept wondering: What’s actually in our drinking water?
So I ordered a lead test. (Hot tip: Tests are free to residents in New York City.)
A few weeks later, the results came back — all within safety limits. But I couldn’t stop thinking about families who might not be so lucky, or may never think to check. Even today, in 2025, tens of thousands of homes across New York are still served by aging lead pipes. Exposure to lead, especially for kids and pregnant women, can cause lifelong harm.
This is why cities like Albany began replacing 2,500 lead pipes (~40% of homes there are still connected to lead pipes), Syracuse is replacing more than 3,000 lead pipes, and Buffalo plans to replace about 40,000 lead pipes. It’s why you’re hearing more about this in the news. And it’s why so many of you asked me to investigate it.
Let’s break down what’s happening, why it’s a concern, and what steps you can take to protect your household.
Lead 101 refresher
Lead is a heavy metal that was widely used in paint, gasoline, plumbing, and construction until the 1970s. After strong evidence showed the dangers of lead exposure, especially among kids, federal and state laws began phasing it out. The 1974 Safe Drinking Water Act was a turning point.
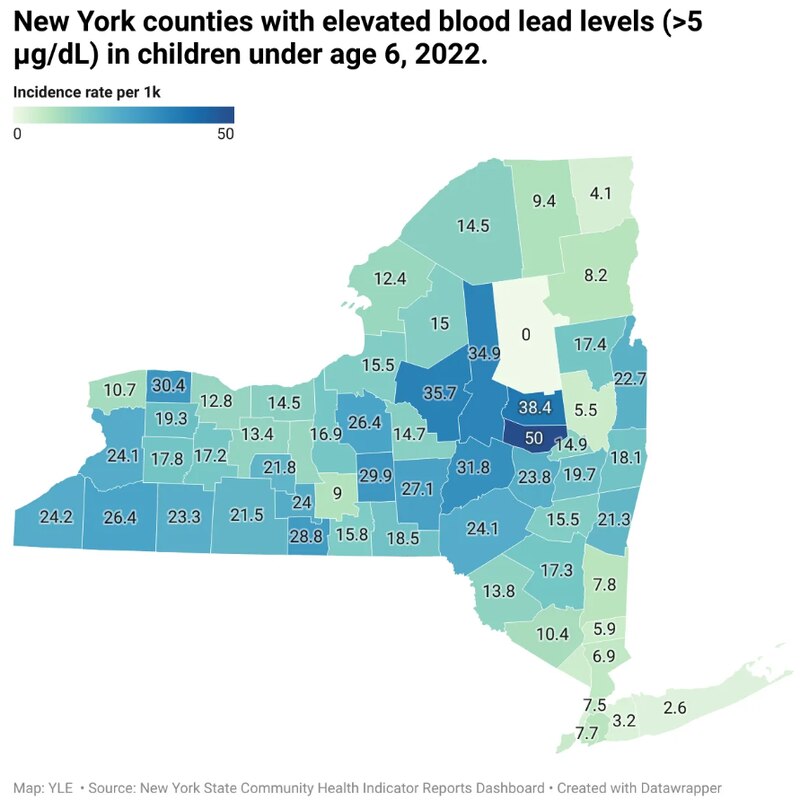
But while we’ve stopped using lead in construction, much of it is still around. Today, too many New York families are still exposed. In Montgomery County, for example, 50 out of every 1,000 children (or 1 in 20) have elevated blood lead levels (above 5 μg/dl). Statewide, about 1% of kids under age 6 had elevated levels in 2022. Above these levels, doctors should pay close attention to a child’s growth and development and screen for any issues.
Lead is especially harmful during critical development windows. Even small amounts can cause:
- Brain and nervous system damage
- Slowed growth and development
- Learning and behavior issues (e.g., reduced IQ, ADHD)
- Hearing and speech impacts
- High blood pressure and brain, kidney, and reproductive health issues in adults
How lead gets into drinking water
Most lead exposure today comes from old lead paint and dust in homes built before 1978.
Drinking water is another potential (though less common) source, as the Flint, Michigan, crisis reminded us.
Lead can enter drinking water in two ways:
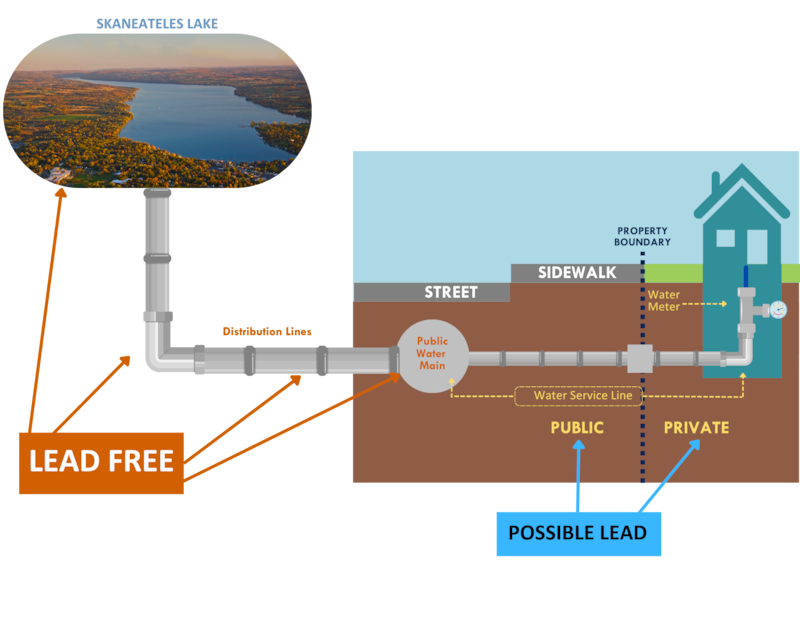
- The source. Public reservoirs in New York are regularly tested and lead-free. Private wells in New York are rarely contaminated with lead at the source, but the Environmental Protection Agency doesn’t regulate them, so homeowners must test their own water.
- The plumbing. This is the bigger problem. Lead can enter drinking water through corroded pipes, faucets, or fixtures, especially in homes built before the 1980s, when lead-based materials were still common. Even with a private well, your home’s plumbing may still pose a risk if it contains lead components.
What the state is doing
Despite lead being banned from new construction decades ago, the legacy of past use remains. That’s why New York is taking several steps to reduce exposure:
- $340 million is being invested to replace lead service lines across New York.
- New York schools must test and fix their drinking water if lead is found.
- Cities, including NYC, treat water with phosphoric acid (a food additive) to coat pipes and reduce lead leaching.
- A new 2025 law will require landlords in 25 New York communities to eliminate lead paint hazards.

Still, much of the burden falls on families — testing their homes, navigating old infrastructure, and making fixes that take time, money, and effort.
What you can do
Lead exposure is a home-by-home issue. Even if public water mains are lead-free, the final stretch of plumbing —especially in homes built before 1986 — can contain lead pipes, solder, or fixtures.
Here’s how to protect your household:
- Test your water. Certified tests cost $15-$50. In New York City, you can request a free kit.
- Use a water filter or bottled water if your drinking water contains lead.
- Use only cold water for drinking, cooking, and baby formula. Run the tap for 30 seconds until it’s cold — this flushes out water where lead may have built up. Boiling doesn’t remove lead.
- Check for peeling paint. If you have young children, report peeling or damaged paint to your landlord. New York City landlords are required to fix lead hazards, and starting in 2025, this will apply statewide in 25 high-risk communities.
- Boost nutrition. Certain foods help reduce how much lead the body absorbs:
- Calcium: milk, cheese, tofu, yogurt, and leafy greens
- Iron: beans, lean meat, fortified cereal, and peanut butter
- Vitamin C: oranges, grapefruit, tomatoes, and peppers
- Get tested. Symptoms of lead poisoning are often silent. That’s why blood testing is the only way to confirm exposure. In New York, doctors are required to test all children at ages 1 and 2, and assess risk through age 6. Pregnant women should be screened at their first prenatal visit. Ask your employer about testing, or talk to your doctor if you work around lead.
Lead exposure is not equally distributed. Children from families with lower incomes are more likely to live in older homes and have elevated blood lead levels. This is another reason why universal screening is so important.
Bottom line
Lead exposure remains a serious but solvable problem. Cities across New York, like Albany, Buffalo, and Syracuse, are removing thousands of old lead pipes, and a new state law will hold landlords accountable for lead removal. You can also take steps, like testing your water, using only cold tap water for drinking and baby formula, and talking to your doctor about lead testing during pregnancy and early childhood. Being aware and knowing what steps to take can help make New York’s homes safer and healthier for everyone.
Love,
Your NY Epi
Dr. Marisa Donnelly, PhD, is an epidemiologist, science communicator, and public health advocate. She specializes in infectious diseases, outbreak response, and emerging health threats. She has led multiple outbreak investigations at the California Department of Public Health and served as an Epidemic Intelligence Service Officer at the Centers for Disease Control and Prevention. Donnelly is also an epidemiologist at Biobot Analytics, where she works at the forefront of wastewater-based disease surveillance.