Public health, explained: Sign up to receive Healthbeat’s Global Checkup in your inbox a day early.
Hello from Nairobi.
The approach of the Thanksgiving holiday is a delightful reminder of just how wildly enterprising Kenyans are. Cranberry sauce and pecans? On the supermarket shelves! Orange pumpkins? Sweet potatoes? A close-enough local fowl called the kienyeji turkey? All at the market right now!
(If you don’t understand my excitement, you may need to endure a few chicken-and-potato holidays before you really appreciate these things.)
My name is William Herkewitz, and I’m a journalist based in Nairobi, Kenya. This is the Global Health Checkup, where I highlight five of the week’s most important stories on outbreaks, medicine, science, and survival from around the world.
With that, as we say in Swahili: karibu katika habari — welcome to the news.
Global climate talks meet health crises
The United Nation’s Climate Change Conference is wrapping up this week in Belém, Brazil, a city at the mouth of the Amazon. Last year was the hottest in our species’ recorded history (again!), so as you might imagine… there is plenty to discuss.
Which is why it’s especially striking that global health policy (generally) and the surge of yellow fever and dengue cases across Amazon-adjacent countries (specifically) found its way onto the main agenda. In fact, the organizers designated Nov. 13 as the conference’s first ever “Health Day.”
As a rule, I try to steer clear of stories that amount to “UN bureaucrats invent a theme day to juice visibility.” But I am making an exception here, because this wasn’t just theater.
As The Guardian reports, the conference and the government of Brazil released an action plan to “help countries … deal with climate-fueled health issues” and a 100+ page roadmap on how to implement that plan. This marks the most serious the international community has ever been about proactively addressing climate change as a force that scrambles global health systems.
The authors (including leading researchers from eight universities) spell out the scale of the issue in a way that’s impossible to ignore. “Climate change is one of the most urgent global health challenges of the 21st century,” they write. “Nearly half the world’s population … live in highly climate-vulnerable contexts, and about 1 in 12 of the world’s 200,000 hospitals faces the risk of total shutdown from extreme weather under high-emissions scenarios.”
What does this mean in practice … and how should we read these recommendations during a moment when global health investments are retracting at their fastest pace in a century? I reached out to Dr. Kristie Ebi at the University of Washington, one of the world’s foremost experts on the health risks of climate change, to help break it down.
The heart of the roadmap is not a list of shiny new, expensive programs. Instead, it is a dramatically unsexy push to make health systems more flexible and more anticipatory.
For example, the authors outline for countries how to structurally reinforce their hospitals and overhaul the power, water, and other systems that keep them running, so they don’t buckle during heat waves or floods. They also spell out how to link climate and health data and train a workforce that can catch climate-driven risks before they spiral. As Ebi noted, “climate change remains relatively new for most ministries of health, with limited internal expertise,” which makes even the basic work of adding climate data to surveillance harder than it looks.
The most difficult part of the plan, Ebi noted, is the future-facing analysis it demands. Plenty of countries have reviewed how climate change could hurt their health systems, but many still don’t have the tools to actually predict what those risks will look like in the years ahead. And that gap is not academic. If a given country’s ministry/department of health cannot anticipate how heat, rainfall, supply chains, or migration will shift over the next decade, they are basically driving without headlights. The roadmap is trying to force a shift away from emergency response and toward planning for the risks that are already coming into view.
And then, of course, there is the money question. Yes, this work is coming at an inopportune financial moment. But the report is blunt that costs will rise sharply the longer countries wait. And Ebi is clear that this is not optional.
“Nearly everywhere experienced extreme weather ... often with devastating consequences. Increasing preparedness to these events will save lives,” she said.
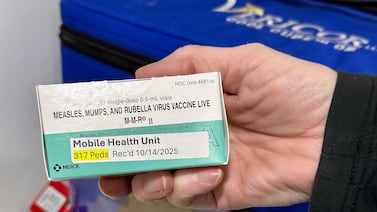
A second cholera vaccine?
Some good news this week: South Africa has begun clinical trials for the first cholera vaccine to be manufactured on the continent, South Africa’s Sunday Times reports.
- Disease breakdown: Cholera is a bacterial infection that infects up to 4 million people each year. Because it largely spreads through water contaminated with feces, it thrives in humanitarian disasters or anywhere else that basic sanitation has broken down. (Think conflict or flooding.) Cholera’s horror is its speed. It causes sudden, violent diarrhea that can empty the body so quickly that stools turn a pale, milky white. Without treatment, cholera can kill in a matter of hours.
The trials are a joint effort between Biovac, a local pharma firm, and the South African government. To be clear, this is not the first vaccine of its kind. A firm called EuBiologics in South Korea makes the only other cholera vaccine. Two doses of that vaccine protect about 70% of recipients for about two years, but … there’s not enough of the vaccine to meet demand.
This shortfall comes as cases rise globally, fueled by overlapping climate shocks and conflicts. It’s a squeeze that Health Policy Watch says “has severely constrained the global supply of cholera vaccines, leading to rationing and global shortages.”
Africa is the hardest hit. The continent is going through the worst cholera outbreak in a quarter-century, with cases surging in countries as disparate as Sudan, Burundi, and Angola, Al Jazeera reports. So this new vaccine is timely.
That said, let me be a realist/downer for a moment. Clinical trials usually move through three phases, and this is only the first one. (Phase 1 is where researchers check basic safety, not even whether the vaccine, uh, stops cholera.) Only about 10% of vaccines make it out of this early stage, but because this is not some brand-new medical advancement, the odds here are likely much higher. Still, there is a long, unsure road ahead.
But the upside is real. Even just myopically, shoring up the cholera vaccine supply will save tens of thousands of lives. But what South Africa is doing here is bigger than one product. During (and immediately after) the pandemic, many multinational pharma companies announced various expansion plans to manufacture drugs or tests on the Africa continent, with many of those plans scaled back since.
Today’s news shows that, just maybe, durable manufacturing gains will come from homegrown institutions.
Marburg virus in humanity’s cradle
Ethiopia has just confirmed its first ever outbreak of Marburg virus after nine suspected hemorrhagic fever cases in the country’s southwest were sent for testing this week, Bloomberg reports.
- Disease breakdown: Marburg virus is functionally Ebola’s first cousin. A very similar high-fatality fever that often leads to hemorrhaging and organ failure. Untreated, about 9 in 10 people who contract the disease will die. The disease exists endemically in bats, allowing it to spread and occasionally spill over into humans. While this is Ethiopia’s first record of the disease, the World Health Organization says the strain matches those seen in past regional flare-ups. There is, unfortunately, no vaccine.
The epicenter of this new outbreak is a town called Jinka, which I last visited in 2022. It is one of the most fascinating places I have ever been. It sits in a region where some of the earliest hominid fossils have been unearthed, and where dozens of strikingly unique Indigenous communities live in close proximity. The town itself is the gateway to the Mago and Omo National Parks, themselves part of a wider UNESCO World Heritage Site because of the extraordinary cultural and ecological diversity. Most relevantly here, I remember the Indigenous peoples’ access to even basic government services being shockingly poor.
The latest news is that containment is underway, and that Ethiopia is reportedly “moving rapidly.” (Although it’s worth noting that the Ethiopian government has its hands full with various other conflicts and crises … some of them directly of Prime Minister Abiy’s own making.)
Here are my biggest questions right now:
Will the outbreak stay limited to this initial cluster, or spiral? As with the Ebola outbreak still wrapping up in the Democratic Republic of the Congo, will emergency appeals for funding be enough? Finally, without a vaccine to provide a robust buffer, how effective will contact tracing and containment be in such an underdeveloped area?
Mind the funding gap, part 2
A month ago, we followed some UK political drama about British donations to the Global Fund: the massive, 23-year-old organization that collects donations from wealthy governments and funnels them into programs that fight AIDS, tuberculosis, and malaria in more than 100 countries.
Back then, the rumor was that the UK, under Prime Minister Keir Starmer, was mulling a 20% cut in the country’s £1 billion pledge. Now it’s been announced that the UK will instead commit £850 million (over $1.1 billion) for the next funding cycle, representing a roughly 15% reduction, The Guardian reports.
While not as bad as the rumors, this is a bit of a gut punch for a few reasons.
First, Starmer’s party is ostensibly the pro-foreign aid face of the UK. (The opposition Conservative Party has promised to further reduce all foreign aid by another two-thirds when next in power.) The fear is that this reduction eases the geopolitical pressure on other leaders. “There is a danger that this drop in its pledge will lead to reductions in other donor commitments, with real risks for people’s lives,” says John Plastow, executive director at Frontline Aids, a global partnership.
Secondly, while the £850 million pledge is still enormous by any standard, the impact of any cut will be directly measured in lives. Per the Guardian article: A previous study showed that “a 20% cut to the overall Global Fund would result in 330,000 additional deaths by 2040 from malaria alone,” let alone the impact on HIV and tuberculosis cases, as the “fund provides 59% of international financing for malaria.” And with malaria cases now surging again in places like Myanmar, after years of decline, the risks of even a modest funding pullback look even starker, the Financial Times reports. (Sorry, paywall.)
It’s still too early to say how this will impact the total funding picture. I’ll be following up next month after the Global Fund closes its “replenishment conference,” the part telethon, part diplomatic speed-date that decides how much money the fund will actually have to work with.
Tuberculosis declined in 2024. Good thing nothing has happened since.
In the fight against tuberculosis, we finally brought a reversal of the pandemic-era spike that interrupted decades of steady declines. New cases fell by about 2%, Euronews reports .
(Why the rise in the first place? The tuberculosis researchers and modelers I’ve spoken with largely blame that Covid-era spike on people increasingly staying indoors — where tuberculosis spreads more easily — and on a diagnostic choke point. Basically: During the pandemic, if you had a bad cough, you got tested for Covid, and if the test came back negative, you were basically told congratulations rather than being screened for something else.)
Unfortunately I can’t, in good conscience, appreciate this as the good news story it should be. Blame the WHO’s reporting bureaucracy or the glacial pace at which governments release their health data, but our global tuberculosis picture is always about 12 months out of date. And this year was a doozy!
Tuberculosis is especially exposed to this year’s global funding crunch, and today’s report warns that “cuts from wealthy countries could lead to up to 2 million additional deaths from [tuberculosis] and 10 million new illnesses over the next decade.”
My read: In all likelihood, the progress we’re seeing in last year’s data has already slipped away in the year since.
We’re off next week, so see you in December!
William Herkewitz is a reporter covering global public health for Healthbeat. He is based in Nairobi. Contact William at wherkewitz@healthbeat.org.