Dr. Jay K. Varma is a special contributor to Healthbeat. Public health, explained: Sign up to receive Healthbeat’s free national newsletter here.
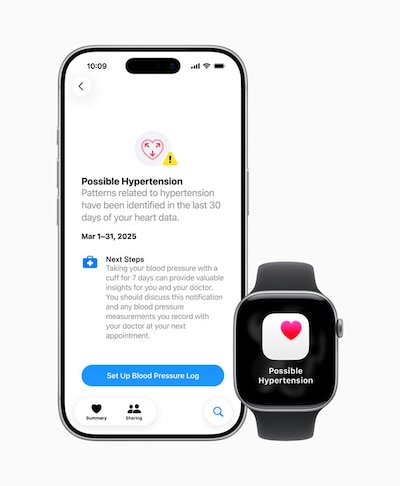
When the Food and Drug Administration cleared the Apple Watch Hypertension Notification Feature this year, it approved a medical device that, curiously enough, does not actually measure blood pressure. Instead of displaying systolic or diastolic readings, it aggregates data from its light sensor and, after 30 days of monitoring, uses a mathematical algorithm to decide whether to alert a user that their blood pressure may be high and could benefit from being checked.
While the Apple Watch identifies only about 40% of people with hypertension, the FDA cleared it because the device’s specificity is high. That is, most alerts indicate high blood pressure, and, for a person who already owns an Apple Watch, there is no additional cost.
When I heard the FDA announcement, I was struck by how it represents a larger shift that has been occurring in both personal and public health. As more health-related data become available, duration can sometimes be more important than accuracy. That is, the longer and more continuously we can monitor patterns, whether in a person’s physiology or a community’s wastewater, the better able we are able to assess health, even if each individual measurement is imperfect.
How technology is changing how we test people for diseases
For most of modern medicine, we designed tests for two different purposes and used them in sequence. We first use tests with high sensitivity — ones that rarely miss disease — to screen a large population. If someone tests positive on this test, we then use a second test with high specificity — one that rarely gives a false positive — to definitively diagnose them with a disease and offer them treatment.
For example, when I was working in Southeast Asia, I helped develop a screening test that could identify people with HIV who were likely to have tuberculosis, the leading cause of death in that population. The purpose of that screening test was to identify patients who would benefit from further testing, such as chest X-rays and microbiologic analysis of their sputum, and, if diagnosed, anti-TB treatment.
As wearable sensors become more available, many of us are concerned that these devices are too sensitive. They will trigger false alarms, leading to unnecessary visits, anxiety, and wasted clinical resources. Apple took a smart approach by adding an additional dimension: What happens if we continuously apply an imperfect test to a person, then aggregate the results of that imperfect test over time before delivering a result?
In some ways, Apple shifted to a “specificity-first” approach for hypertension: missing some cases temporarily is acceptable, because confirmatory testing is cheap (a blood pressure cuff), the condition develops slowly, a delay in diagnosis is rarely deadly, and the monitoring runs constantly in the background. It also helps prevent monitoring fatigue, i.e., people ignoring alerts because the device is constantly indicating something is wrong.
The Apple Watch has an optical light sensor that detects changes in light absorption due to pulsatile blood flow. When combined with motion and heart rate data, the watch’s software detects patterns that suggest sustained high blood pressure.
In the studies Apple conducted to get approval, participants wore the device for at least 15 days within a 30-day window. The algorithm correctly identified high blood pressure in about 40% of adults who truly had the condition, while falsely indicating high blood pressure in 8% of adults who did not have the condition. Among people with Stage 2 hypertension, over 50% were correctly identified.
While this means that half of people with high blood pressure will not be detected, the algorithm was deliberately designed to minimize false positives while ensuring that the highest-risk users were the most likely to receive alerts. In this model, the objective is to identify people at highest risk and push them toward having a definitive test. Moreover, it is assumed that people with hypertension who are missed during one screening period might be detected at a future date if they continue wearing the watch. Continuous monitoring helps compensate for imperfect snapshots.
While clinical medicine has used continuous monitoring to measure abnormal heart rhythms and changes in blood sugar, Apple and other companies are creating devices that are worn for non-health purposes by millions of people already while also collecting health data passively and unobtrusively.
How continuous monitoring has benefited public health practice
What Apple is doing for individual health has been something that public health has been gradually shifting toward as well. For most of modern public health, our disease surveillance systems have relied on discrete moments, such as laboratory tests or household surveys. Two big infectious disease events changed that.
After the bioterrorism-related anthrax attacks in 2001, public health agencies began implementing syndromic surveillance systems. Instead of tracking laboratory or physician reports of disease, public health agencies began monitoring health-related events, such as 911 calls, emergency department visits, and over-the-counter medication sales. These data were messy and nonspecific, but the fact that they were collected continuously over years made them powerful. In late February and early March 2020, this data indicated a rise in “influenza-like illness” visits to emergency departments after peak influenza season. This was a trigger — just like an Apple Watch hypertension alert — to test for other pathogens, such as Covid, which had not yet been detected broadly in the community.
The Covid pandemic led to another shift in continuous monitoring: wastewater surveillance. Wastewater contains genetic fragments of viruses and other pathogens excreted by infected persons, including those who have not yet been diagnosed. Microbiologists are able to test wastewater specimens to detect and follow trends for infectious diseases that may be circulating in the community. Any one test performed on a sewage specimen is unlikely to be useful, because it contains the waste of many humans and animals, but continuous tracking from multiple sites in cities has helped improve detection of Covid before standard surveillance did.
Opportunities for continuous monitoring to improve public health in the future
The same principle now extends to other domains where continuous monitoring can help turn “noisy” data into important health signals.
Efforts are ongoing to expand wastewater surveillance to monitor a broader range of pathogens beyond Covid, such as mpox and measles, and for opiates and other illicit drugs.
New devices can listen for cough and collect data continuously to help monitor for an increase in respiratory infections, including seasonal viruses and TB.
Public health agencies primarily rely on periodic surveys of children and of school entrance records to monitor vaccination uptake. With anti-vaccine sentiment rising, these episodic measurements may miss early trends in vaccine hesitancy or refusal that might be detected earlier by aggregating electronic health record data.
We still need highly accurate laboratory tests
Continuous monitoring needs to complement, rather than replace, traditional public health surveillance, such as laboratory-reports of confirmed cases. The first tells us that something may be happening; the second tells us what is definitively happening and how to respond.
This is particularly important for high-consequence infectious diseases — like novel influenza strains, measles, botulism, or Ebola — in which public health officials and clinicians need tests with both high sensitivity and high specificity. In these settings, a single false positive can lead to unnecessary interventions and public concern, while a false negative can delay opportunities to limit transmission.
Challenges for monitoring health continuously
Constant monitoring of individuals and populations creates new ethical and equity challenges. Wearable devices generate massive streams of physiological data. Questions remain about ownership, consent, and potential misuse by employers or insurers. Algorithmic bias also threatens fairness. Apple says it invested in large, diverse clinical studies to validate performance across skin tones and demographics, but we know that devices may not work the same in all populations. Portable oxygen monitoring (“pulse oximetry”) was used for 40 years before a large study showed definitively that it produced inaccurate results in people with dark skin tones.
Continuous observation is transforming how we understand both individual and population health. Wearables like Apple’s hypertension feature for individual health and wastewater surveillance for public health share a common principle: While a single data point may be “noise,” a pattern across thousands of data points may be a “signal” for action. The future of public health surveillance will ideally include a combination of both more accurate individual tests and broader sources of data to detect patterns that might otherwise be missed.
Dr. Jay K. Varma is a physician and epidemiologist. An expert in the prevention and control of infectious diseases, he has led epidemic responses, developed global and national policies, and implemented large-scale programs that saved hundreds of thousands of lives in Asia, Africa, and the United States.