Public health, explained: Sign up to receive Healthbeat’s free Atlanta newsletter here.
The Fulton County Board of Health this week laid off 17 workers, including those focused on HIV and sexual health services, apparently without the approval of the state Department of Public Health.
The unexpected layoffs prompted the state to place “two executive leaders” of the county agency on unpaid administrative leave.
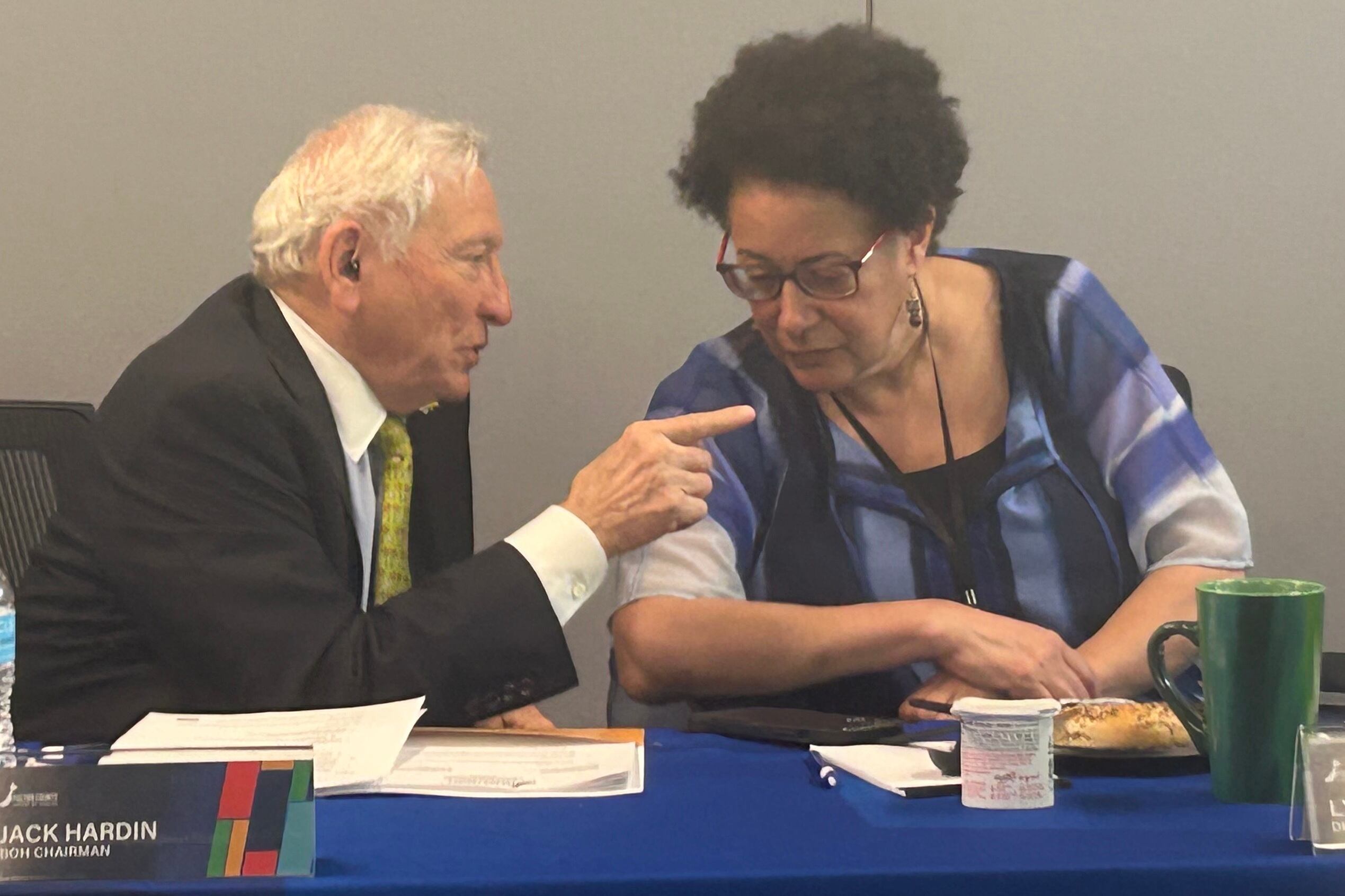
Jack Hardin, chairman of the Fulton health department’s board, confirmed Wednesday that District Health Director Dr. Lynn Paxton and Human Resources Director Carol Lawrence were placed on leave. Chief of Staff Brian Easom is leading the department.
The Monday layoffs “were done without the prior knowledge or approval of the Georgia Department of Public Health,” spokesperson Nancy Nydam said Wednesday in an email, and “DPH is reviewing the actions.”
Neither Paxton nor Lawrence could immediately be reached for comment.
Hardin said the layoffs were part of a restructuring and would not affect delivery of services.
“FCBOH emphasizes there is no disruption in HIV, STI, and TB clinical services because of these actions,” Nydam said.
County health departments like Fulton’s provide a range of HIV testing and other sexual health services.
Tyson Randolph, who told Healthbeat he was laid off on Monday, said his team was working on innovative ways to bring services to those who aren’t typically reached.
He worked on public health education with youth groups and college students in Atlanta’s West End, where he lives.
The layoffs will have “major implications for the community’s health going forward,” Randolph said. “I was in the developmental process of building the bridge with the kids at this community center … but my efforts are all out the window.”
HIV testing services are vital in metro Atlanta. Fulton, DeKalb, and Clayton counties were among the 15 counties with the highest rates of new HIV diagnoses in 2022, according to the latest available data from AidsVu.
The U.S. Centers for Disease Control also recently laid off much of its HIV prevention staff, including the team working on preventing mother-child transmission of the disease. A CDC-funded program headquartered at Emory University that delivered nearly 750,000 free home HIV testing kits also will be canceled.
Community groups across the South have cut back on HIV services due to funding delays and cuts.
The Fulton County workers laid off this week will be paid through the end of May, with additional severance payments in June, according to a letter to one employee viewed by Healthbeat.
The staffing cuts come after the state health department lost an estimated $334.2 million in funds due to “clawbacks” of Covid-era funding from the CDC announced in March. Those cuts resulted in layoffs of temporary contact tracers and other workers at the state agency.
Georgia community groups including those focused on vaccine outreach and equity also lost grants due to the cuts.
This story has been updated to correct a quote from state health department spokesperson Nancy Nydam to include that the Fulton County Board of Health emphasized that HIV, STI, and TB clinical services would not be disrupted.
Rebecca Grapevine is a reporter covering public health in Atlanta for Healthbeat. Contact Rebecca at rgrapevine@healthbeat.org.